Table of Contents
You can click a link to be taken directly to the highlighted content.
Overview
Care Coordinator Steps
Step 1: Recieve Positive Screen Notification
Step 2: Review Patient Information
Step 3: Notify PCP that a Positive Screen was Received
Step 4: Reach Out to the Patient in the Portal
Step 5: Provide Services for Referrals and Treatment
Step 6: Let PCP Know Patient's Update
Step 7: Check Patient was able to Access Resources
Step 8: Ongoing Care Coordination
Step 9: Closing Patient Out
Screens
PHQ-9
Goals and Mission of Mammha
Mammha was created to ensure finding care is easy for both providers caring for perinatal women, and women who are experiencing a maternal mental health complication, such as depression and anxiety. We created Mammha so that no woman has to do this alone, or struggle to find her own way. Mammha creates a system whereby doctors are supported when they ask women how they are feeling, and those women are provided better, faster support.
With Whom does Mammha Work?
Mammha works with OB/GYNs, pediatricians, neonatologists, occupational therapists, midwives, nurses, social workers, Advanced Nurse Practitioners (APRNs), and doulas. We also work with mothers, families, and therapists.
How Mammha Works
1. Providers Initiate Screens
Provider initiates a screen using a QR code, screening link, or patient information sheet
Mom can screen in the office, hospital, or remote
The provider can be an OB, Pediatrician, Neonatologist, hospital social worker, Occupational Therapist, nurse, office receptionist, midwife, APRN, or Home Visiting Nurse
2. Patient Screens
Using her phone, laptop, or in-office tablet, user takes the screen
Screen is the Edinburgh (EPDS)
3. Results to Patient
User receives a results message:
If Negative:
She receives education and follow-up automatic text that she can reach out to get support discreetly, if needed
If Positive:
She receives a link with her mom portal that is filled with multiple low to no-cost resources.
She receives a message that her Mammha Care Coordinator will be reaching out to her within 24 hours.
She is signed up for 90 days of automatic SMS messages
If High:
She receives an emergency message informing her that if this is an emergency to call 9-1-1, or to reach out to the Suicide Prevention Lifeline
She receives a link with her mom portal that is filled with multiple low to no-cost resources
She receives a message that her Mammha Care Coordinator will be reaching out to her
She is signed up for 90 days of automatic SMS messages
If Positive for Thoughts of Self-Harm:
She receives an emergency message informing her that if this is an emergency to call 9-1-1 or to reach out to the Suicide Prevention Lifeline
She receives a link with her mom portal that is filled with multiple low and no cost resources
She receives a message that her Mammha Care Coordinator will be reaching out to her
She is signed up for 90 days of automatic SMS messages
4. Results to Provider
Provider who initiated the screen receives an SMS notification and email informing them that their patient completed the screen.
Provider receives enhanced screen results which include:
Mom’s score for screen
Mom’s answers to the questions on screen
Talking points
Triage phone numbers
5. Results to Mammha Care Coordinator
Mammha Care Coordinator is notified via SMS and email if a patient from the office they have been assigned has screened positive, high, or positive for thoughts of self-harm.
Care Coordinator receives enhanced screen results which include:
Score
Answers
Talking points
Triage phone numbers
Mom’s insurance provider
Pregnant or postpartum
Name of baby and birth date
If mom was in office or remote
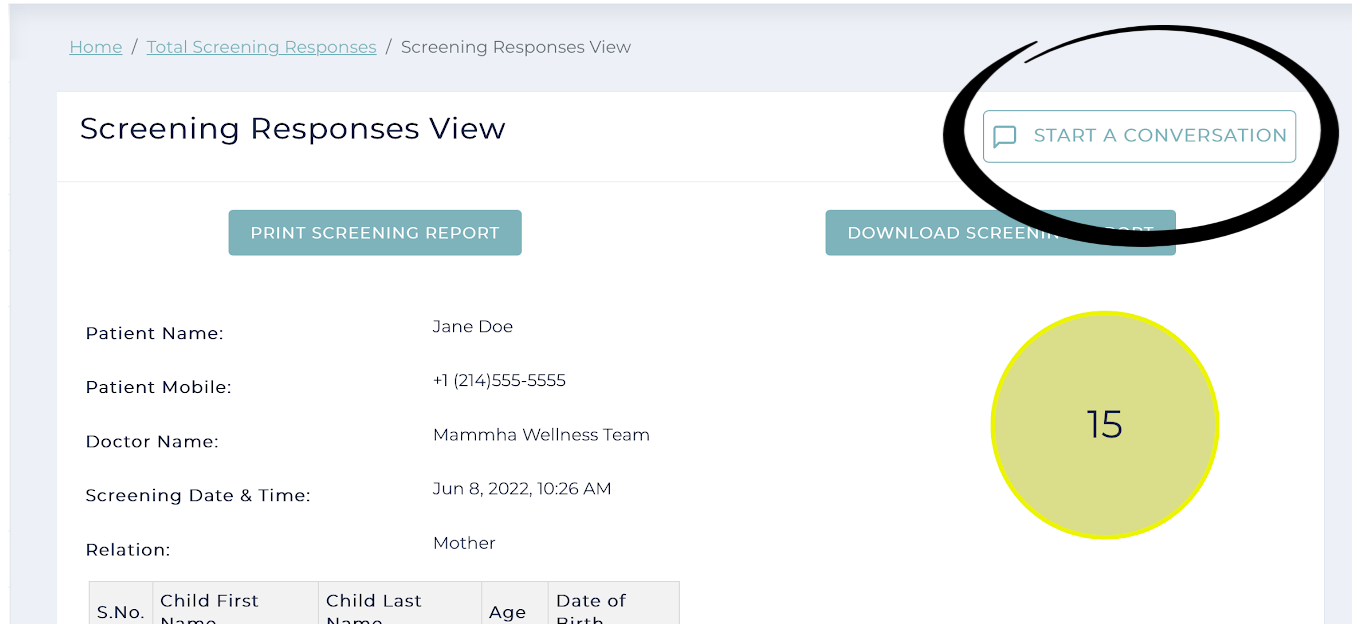
Care Coordinator has a button attached to the patient’s screen record to initiate communication with the positive-screened mom from the Care Coordinator portal
What is a Mammha Care Coordinator?
Mammha Care Coordinators are a mom’s lifeline. They help moms access care, feel supported, and they circle back to physicians and providers to inform them that patients have been contacted, and any follow-up steps that need to be taken by the Care Coordinator. For example, connecting her to a therapist, or inviting her to mom groups every week.
How Mammha Care Coordinators Communicate with Moms
98% of communication is through text messages
2% will request to talk by phone for the first contact, with follow-up communication via text message
Types of Responses from Moms to Care Coordinators from Initial Contact
10% never engage with their Care Coordinator
No response to 3 attempts of contact
5% engage one time
Mom may respond to let you know text is best, then the Care Coordinator gives resources, and may not hear back from mom.
They express to you that their anxiety is normal
They express that they already have a mental health team, and do not require follow-up services
85% engage more than 2 times
These moms stay connected on average for 6 weeks
Screen Scores
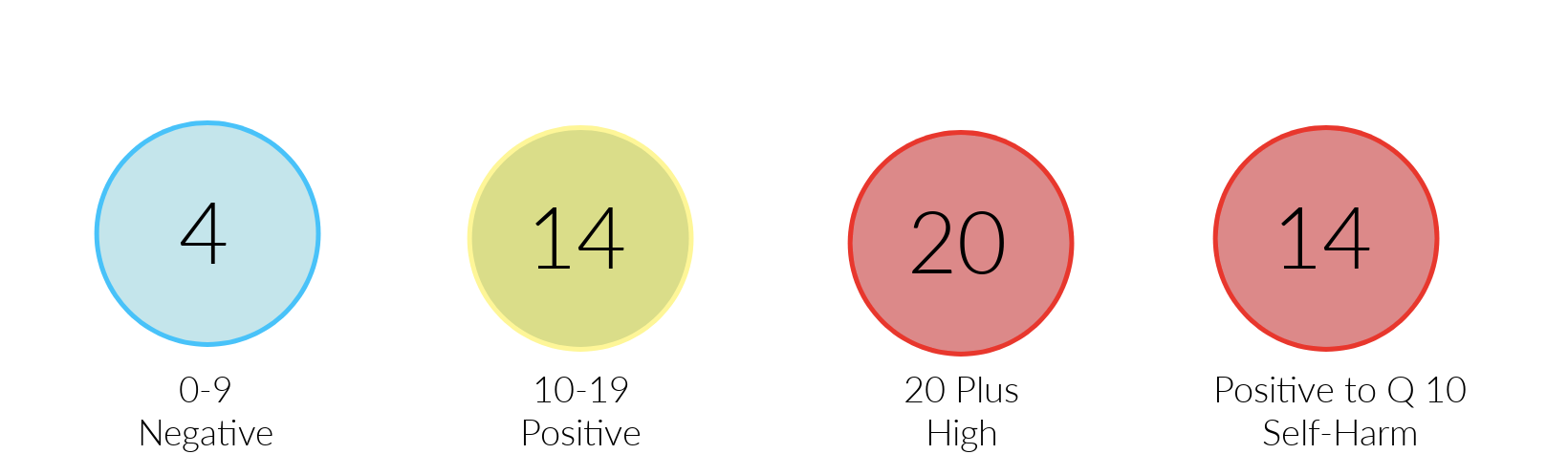
Mammha uses two screens, one for pregnant and postpartum patients, and one for non-perinatal patients. The two screens Mammha uses are the EPDS and the PHQ-9. EPDS
EPDS
Mammha uses the EPDS screen for perinatal patients and the PHQ9 for non-perinatal patients. Below are the score cut-offs for perinatal patients.
0-9 = Negative
10-19 = Positive
20+ = Positive High
Yes to Question 10 = At Risk for Self-Harm
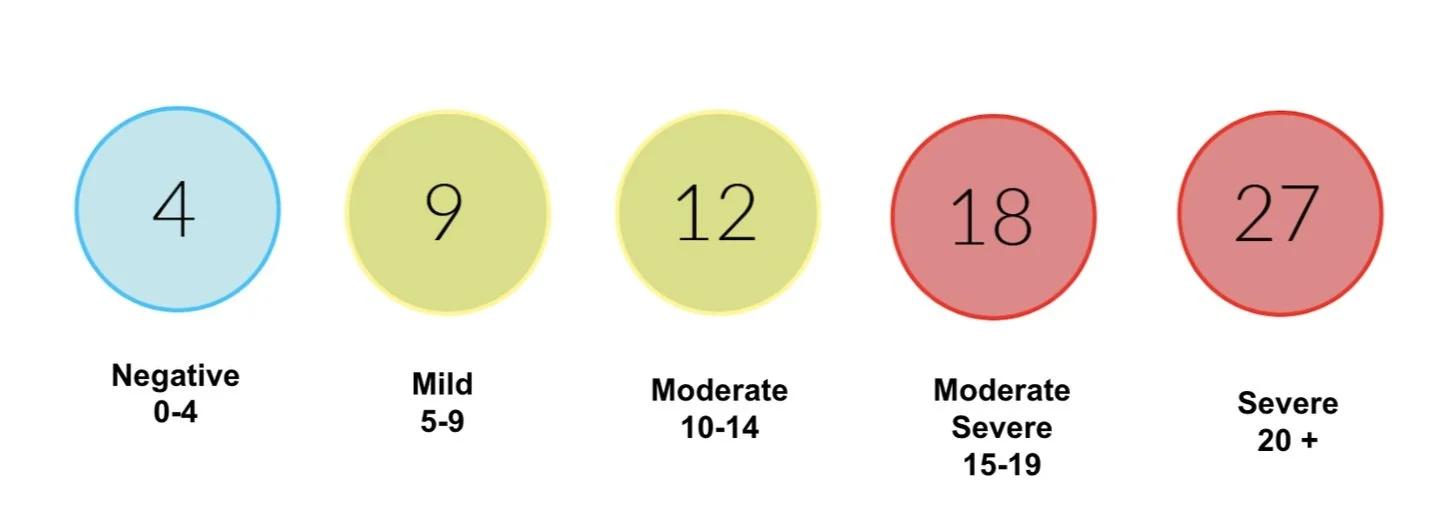
PHQ-9
Mammha uses the PHQ-9 to screen non-perinatal patients, these are patients who are non-pregnant and have not had a baby in the last year. Below are the score cut-offs for perinatal patients.
0-4 = Negative
5-9 = Mild
10-14 = Moderate
15-19 = Moderate Severe
20+ = Severe
Response Times
You have 6 hours to respond to mom, but sooner is better. Remember what it was like for you. So try to respond to her via text in your Care Coordinator portal within 1 hour.
Positive Screen, 10 - 19 on EPDS
When a patient screens positive, 10-19 score on their EPDS, attempt to reach her a total of a minimum of:
3 times within 72 hours
You have up to 6 hours to reach out for the first time, the goal is within 1 hour.
We prefer the first response to be within the first hour after screening positive. For this first response, you can send a text message to introduce yourself (see below on proper protocol).
If she does not reply after the first attempt, reach out again 24 hours later. This time by calling her on the phone. If she does not respond to your phone call. Let the provider know and ask them if they can let the mom know you are trying to reach them.
Try again, 72 hours after she screened positive, this can be via text or phone. If no response on the third time, let the provider know.
At this point, we like to send several more texts for an additional 2 to 3 weeks with updates on support groups, a gentle reminder that you are there if they need any support and that if they ever feel they want to speak to a therapist, you are there to help.
High Screen 20 Plus on EPDS
When a mom screens high positive, 20 plus on her EPDS, attempt to reach her a total of:
3 times within 48 hours
You have up to 1 hour to reach out for the first time. We prefer the first response to be within 10 minutes after screening high positive. For this first response, you can text first to let her know you are going to call her on the phone. Then call on the phone to speak to her.
If she does not reply after the first attempt, let the provider know if they can let the mom know you are trying to reach them.
Try to reach them again 24 hours later, by phone and text. If no response, again, let the provider know you haven’t been able to reach them and can they help.
Attempt to reach out again via phone and text, 48 hours after screening. If no response on the third attempt, let the provider know.
At this point, we like to send several more texts for an additional 2 to 3 weeks with updates on support groups, a gentle reminder that you are there if they need any support and that if they ever feel they want to speak to a therapist, you are there to help.
Positive to Thoughts of Self-Harm (Question 10 on EPDS)
When a mom screens positive to thoughts of self-harm, positive on question 10 on the EPDS, attempt to reach her a total of:
3 times within 48 hours
You have up to 1 hour to reach out for the first time. We prefer the first response to be within 10 minutes after screening yes to question 10. For this first response, you can text first to let her know you are going to call her on the phone. Then call on the phone to speak to her.
If she does not reply after the first attempt, let the provider know if they can let the mom know you are trying to reach them.
Try to reach them again 24 hours later, by phone and text. If no response, again, let the provider know you haven’t been able to reach them and can they help.
Attempt to reach out again via phone and text, 48 hours after screening. If no response on the third attempt, let the provider know.
At this point, we like to send several more texts for an additional 2 to 3 weeks with updates on support groups, a gentle reminder that you are there if they need any support and that if they ever feel they want to speak to a therapist, you are there to help.
Step 1: Recieve Positive Screen Notification
Step 2: Review Patient Information
Step 3: Notify PCP that a Positive Screen was Received
Step 4: Reach Out to the Patient in the Portal
Step 5: Provide Services for Referrals and Treatment
Step 6 Let PCP Know Patient's Update
Step 7 Check Patient was able to Access Resources
Step 8 Ongoing Care Coordination
Care Coordinators Reaching Out to Moms
Mammha Care Coordinator Interaction with Mom
Average interactions are 63 text messages (that is total number back and forth)
The least amount of interactions to-date has been 7, and the highest has been over 370
Interactions can be a duration of 2 weeks or up to 9+ months, depending on the mom
Average length of interaction is 6 weeks
Roles of a Mammha Care Coordinator
Helps connect moms with therapists
Invites moms to support groups
Checks in on her
If the mom starts taking medicine, checks in on how she feels with the medicine
Speaks to family members on her behalf
Celebrates when she is feeling better
Gives her hope when she is feeling down
Provides resources such as articles, tools, and podcasts
Follow up within 24 hours to the provider to inform them whether contact was made
Checking in on Moms
One of the most important things a Care Coordinator does is provide regular check-ins on moms.
There is a metaphor that says a postpartum woman is just like a wrapper around a piece of hard candy. Imagine the baby as the piece of hard candy, and mom is the wrapper. When the baby is born, our society and medical system tend to throw the wrapper away.
Check-ins are more frequent after she first screens positive, or if she is having a hard time.
Below is the recommended check-in schedule which begins right after she screens positive, and when the first contact is initiated.
Week 1:
Check in 3 times
Week 2:
Check in 2 to 3 times
Week 3:
Check in 2 times
Week 4:
Check in 2 times
Week 5:
Check in 1 time
Week 6:
Check in 1 time
Week 7 or More:
If mom needs more support, use judgment and/or check in weekly
Check-Ins
When checking in on mom, ask open-ended questions to find opportunities where she can best be supported.
Some easy go-to check-in questions are:
How are you feeling today?
How is your anxiety?
How are you sleeping?
On a scale of 1 to 10 how is your mood this week?
How is the baby feeding?
How is the pregnancy going?
How is your support system?
How are you eating?
Have you been drinking plenty of water?
Are you taking any time for yourself?
How is the medicine making you feel?
How was the visit with your in-laws?
How was the doctor appointment?
Check-in Message to Mom:
Good Morning (Name of Mom), I wanted to check in–how are you feeling today?
These check-in questions help Care Coordinators learn so much about mom, and serve as starting points to go deeper and support her more comprehensively. The goal is to help mom feel better as soon as possible.
It is important to allow her the opportunity to share all of her thoughts and feelings. The act of having someone deeply listening helps relieve the feeling of loneliness and isolation.
Examples:
How are you sleeping? How many hours of sleep are you getting?
With this question we want to see how many hours of sleep she is getting a night
Sufficient sleep is a vital factor in reducing depression and anxiety. The recommended number of hours of sleep a postpartum mom gets, who has risk factors or who is experiencing depression or anxiety, is 4 to 5 hours of uninterrupted sleep. This is the goal.
Many times moms will say, “I slept 2 hours here and there.” That is a red flag.
Some moms will say, “1 hour,” and that is an even bigger red flag.
Sleep deprivation is like a form of torture, and if a mom already has risk factors, or is not feeling great, this is like gasoline on a fire.
Try to help her figure out a better sleep schedule.
Example:
“Is it possible for you to go to sleep a little earlier? Like 8 pm?”
If she has a partner, inquire whether they are able to take the baby until that first midnight/1 am feeding, so she can sleep
If the baby keeps her up because she hears every noise and she cannot sleep, ask her if she can sleep in a different room for a little while to see if she gets better sleep.
If she is extremely sleep-deprived, try to help her figure out if there is someone in her support system who can come and watch the baby while she sleeps.
Ask questions about her sleep habits.
“Can you make the room darker?”
Sleep medications: make sure she knows she can reach out to her doctor if her sleep is not improving; there may be something else she can take.
A Care Coordinator is concerned about sleep psychosis which can occur from lack of sleep for several days. If mom is not sleeping for days, ask if it is ok to speak to her partner, or a family member to discuss how important it is for her to sleep.
Another example:
How is the baby feeding?
Some common responses to this question are: “It has been really hard,” “The baby cries all of the time.” “It has been painful/frustrating.” From here she may start to share how this makes her feel like a failure as a mom.
At this point, it is important to validate her feelings by saying something like: “It must be hard and frustrating.” “So many moms have a hard time. We think it is supposed to be easy and magical because it is natural, but the truth is it can be hard.”
If you have a personal experience with this, you can share it with her so she knows she is not the only one.
Let her know that “fed is best.”
If she is interested in continuing to try to breastfeed, Inquire if she has connected with a lactation consultant.
If she says she has low supply let her know there are teas that can help. Also ask if she is drinking enough water.
Look up La Leche League and find a support close to her to whom she can reach out.
Difficulty with breastfeeding is a big trigger for many women. Remember, the role of a Care Coordinator is not to push her to stop or keep going. Your role is to:
Support her
Listen to her
Validate her feelings
Let her know she is a great mom although this is hard
Let her know that you can help find her some resources to help
Connecting Moms with Therapists and Mental Health Providers
Mammha Care Coordinators help connect moms to a therapist and mental health provider.
The following are guiding principles when connecting a mom to a therapist and mental health provider:
It is important to connect her with a therapist and mental health provider who accepts her insurance unless she says differently.
It is important to connect her with a therapist and mental health provider who matches her cultural and gender preference.
To close gaps, Mammha Care Coordinators try to help schedule the first session or initiate first contact with the therapist and mental health provider on behalf of the mom. Make sure to get permission from mom to share her contact information.
To ensure gaps are closed, Mammha Care Coordinators follow up to make sure mom and the therapist and mental health provider have connected and that sessions have been made.
We suggest letting mom know that you will follow up after she starts seeing the therapist and mental health provider to make sure it’s a good match. You can let her know that if it isn’t a good match, you can help find her a better match.
Below are some questions, or ways to ask about her preference:
Below are some questions, or ways to ask her if she wants to see a therapist:
“Would you like to talk to someone? I have several therapists who specialize in working with pregnant moms (if pregnant), postpartum moms (if postpartum), new moms, or moms experiencing loss.”
If she says “yes,” ask, “Do you prefer a therapist who speaks a particular language, or is from a certain cultural background?”
“Do you have any times that are more preferable to you?” (This is especially important to mention to pregnant or postpartum women who are back to work.)
“I can reach out to see if the therapist or therapists I am thinking about would be a good match, and whether they have openings.”
If she says yes to a therapist:
Use this website to search for a therapist: https://psidirectory.com/
If a therapist cannot be found on that site, use this site instead: https://www.psychologytoday.com/us
Search by state, insurance provider, specialty, and languages spoken, among other search criteria.
If there is a therapist who matches the mom’s preference, select the envelope icon in the right corner of the therapist's profile to send them a message.
In the message, inform them you are searching for a therapist for a pregnant or postpartum mom, who lives in a certain state, and who is experiencing either depression or anxiety. Inform them that she has a specific insurance, and is interested in getting support. Inquire if the therapist has openings, and ask if they accept her insurance.
Example of Message to the Therapist:
Dear (Therapist’s Name),
I am looking for a therapist for a pregnant mom who is experiencing anxiety. She has Cigna insurance and is interested in working with a therapist. She lives in Florida. Do you still have any openings, and do you still take Cigna insurance?
Thank you so much,
(Your Name)
Remember: do not use any personal, identifiable information such as the mom’s name, unless she gives you permission.
If the therapist responds “yes,” inform them that their information will be shared with the mom.
COMING SOON! In the near future, Mammha will have its own therapists. Helping a mom connect with a therapist will be even easier. You will have access to the therapist's schedule and can assist the mom book her first session.
Giving the Therapist’s Information Back to Mom
Inform Mom
Example of Message Back to Mom:
“I have great news! I have heard back from the therapist. Here is her phone number (include the contact number). Here is her website (include the therapist’s website, if applicable) She specializes in working with moms (if this is true) and/or (trauma) (or whichever topic this mom needs most). She has openings and accepts your insurance. You can reach out to schedule your first session.”
Always let her know you will be checking in on her to make sure it is a good match.
Message You Will Be Checking Back In:
“ I will check back with you to see if it is a good match. If it is not, I will help you find a better match. I’m here for you.”
Follow Up with Mom about Making First Session with the Therapist - first time after therapist’s information is sent:
A Care Coordinator is there to ensure that mom gets her first appointment with the therapist.
Always check back in the day after mom is given the therapist's contact information.
Message Checking Back on First Therapist Contact:
“Good Morning/Afternoon (Name of Mom), I wanted to check in to see if you were able to reach (Name of Therapist). Were you able to reach her?”
This message will determine if mom initiated contact, and if the therapist has responded to her.
There are situations when the mom has not reached out yet, and that is ok. It is a nice, gentle nudge for her. The majority of the time, she will inform the Care Coordinator when she plans to call.
At this point, offer, if she is interested, to reach out to the therapist to share her information. Inform her that this can help take something off her plate, and you can reach out on her behalf. A Care Coordinator must first ask for permission to share her contact information.
Message About Reaching Out To Therapist for Her:
“Would you like me to reach back out to the therapist to share your contact information? This way I can help take something off your plate. I know your hands are so full right now.”
If mom says she called and left a message but has not heard back:
There will be times when the therapist does not return the mom’s call. If this is the case, this is where the Care Coordinator plays a pivotal role in closing this gap. (This is your rock star moment! It is where most women slip through the gaps, but not on your watch!)
If mom did reach out to the therapist and is still waiting to hear back, let her know you will contact the therapist to inform them that the mom is still very interested in working with her (the therapist), and she is waiting to hear back.
Ask if it is ok to share mom’s contact information with the therapist at this point.
If mom says yes, share the mom’s name and phone number with the therapist.
If the mom says she prefers not to share her contact information, then communicate with the therapist that there is a mom who recently called and left a message. Stress that this mom would like a return call as soon as possible.
Most moms say it is ok to share their information at this point, because they have already shared their information with the therapist either through email or voicemail.
Follow-Up Phone Call or Email Message To Therapist with Mom's Permission to Share Contact Information:
Hi (Name of Therapist), I spoke with (Name of Mom) and she wanted me to share her phone number with you. It is (phone number). She would love to work with you. She gave me permission to share her information.”
If you communicate with the therapist on the phone, or via email,you will likely receive a response such as: “I will reach out to her today.”
After this exchange, communicate with mom to let her know you heard back from the therapist, and they said they will be calling her today.
Make sure to check in to see if the therapist called.
If the therapist still has not responded, inform the mom that you will look for a new therapist ASAP, and never reach out to that therapist again.
Follow-Up Phone Call or Email Message To Therapist With No Identifiable Information:
Hi (Name of Therapist), The mom mentioned to you before said she tried to contact you yesterday, but has not heard anything back yet. I am just following up. She would really love to work with you.”
If There is a Long Wait for First Session:
We do not want her waiting too long. An appointment available 3 weeks out is not ideal. The sooner, the better.
If the therapist says that their first appointment is in 3 weeks, it may be best to look for another therapist, if mom really needs to see someone sooner. Keep that appointment and look for another therapist, unless she really wants to work with this particular therapist. Be sure to offer her extra support over the next couple of weeks, and set her up with some support groups.
Follow-Up on Therapist After Her First Session
This follow-up determines how that first session went. It also sends the message that you are actively following up. If mom feels like this therapist is not a great match, she will be more comfortable letting her Care Coordinator know.
Follow Up Message To Mom:
“I am just following up. How was the first session?”
Moms should give it at least 2 sessions, but sometimes they know right away if it was not a good match.
If it was not a good match, work to find her another therapist.
If the session went well, continue to check in on her to make sure it is still good.
Follow-Up Message To Mom’s Response on First Therapy Session (if it was OK):
“I’m glad you were able to get that first session in. When is your next session? Just know, I will continue to make sure it’s a good fit and don’t hesitate to reach out if you think you would like to work with someone else. That is what I’m here for.”
Connecting Patients to Support Groups
Groups can be extremely healing for women, especially if they are feeling like they are the only mom out there who is feeling this way. Support groups are also great interventions for women who may have a 2 week wait to see a therapist.
Chose at least one or two groups to share. Let her know the day and time the group meets, if there is a physical location or a virtual link. Instructions on how to register. Always let her know that she never has to participate, she can always listen and if she ever finds a group to be triggering she can leave if it’s in a physical location or log off if it’s a virtual group.
** It is important to note that some women do not like support groups and that is ok. Some women may find the groups very triggering. This is especially true for women who are experiencing intrusive thoughts. It is good to figure out if a mom would benefit from a group by asking her questions on what she is feeling.
To search for relevant support groups
You can search Mammha’s List of virtual support groups: www.mammha.com/mammha-other-support-groups
Or you can search Hey Peers for upcoming Postpartum Support International support groupshttps://heypeers.com/meetings
If you share a Postpartum Support International support group from the hey peers website, always let mom know that these groups fill fast. Let her know it’s best to register early even if she isn’t sure she is going to make it, just to ensure that she will have a spot reserved in case she does want to join.
Let her know, that to register for her first hey peers groups, she needs to first register with hey peers using this link: https://heypeers.com/members/sign_up
After she registers with hey peers, she can use the invite link to the group you share to register.
Inviting Patients to Support Groups As Part of On Going Support
An invitation to a support group is a great way to continue supporting and checking in with mom. Finding a group that meets her unique needs, that has space, that takes place during hours she has available, and that is easily accessible is a way to provide ongoing support to mom.
An easy way to let mom know about upcoming groups is to reach out every Monday, sharing a group or two that is coming up that you think she may be interested in joining. Inviting Moms to Support Groups
One of the special things Care Coordinators do is invite moms to participate in support groups. Groups can be extremely healing for women, especially if they are feeling like they are the only mom out there who is feeling this way. Support groups are also great interventions for women who may have a 2 week wait to see a therapist. It is important to note that some women do not like support groups and that is ok. Some women may find the groups very triggering. This is especially true for women who are experiencing intrusive thoughts.
During the first week of conversations with a mom, always make sure to invite her to at least one support group.
Normally, this is the Mammha Support Group that is on Fridays at 11 am EST.
Invitation to First Mammha Support Group Message:
“Good Morning (Name of Mom), I wanted to make sure you know about our mom group this Friday at 11 am EST. We would love to have you there. Moms find it so helpful to hear they aren’t alone. You don’t have to share. If it feels more comfortable to listen, then you can just listen. Babies are welcome, dogs too. We have pregnant moms as well (if it is a pregnant mom). Here is the link to register: https://www.mammha.com/virtual-support-groups
An invitation to a support group is a way to continue our communication with mom in weeks 4 - 6 for check-ins.
An example of a check-in to invite mom to support groups:
Invitation to Mammha Support Groups After the First Invite Message:
“Good Morning (Name of Mom), We have our mom group today at 11 am EST. We would love to have you!”
There are other support groups we offer moms, depending on what would best benefit them.
At least once a week, especially in the beginning (during the first 3 weeks), make sure to invite moms to the Mammha support group, and depending on the mom and her circumstances, invite her to one of the other special groups listed above.
Providing Resources to Moms
Care Coordinators should share articles, resources, podcasts, tools, websites, and groups with moms.
Podcasts
Podcasts are great resources to share. One of the most popular is Mom and Mind by Dr. Kat. Search “Mom and Mind” and then a particular topic such as rage, loss, and/or depression, to find a specific one to share with mom. Here is the link to these podcasts:
The following are some of Mammha’s favorite topics from Mom and Mind to share with moms:
Podcasts By Black Moms:
Black Mom Healing Podcast
Apps
Canopie App - Free
Free app with CBT techniques and tools
Mindful Mamas
https://www.mindfulmamasclub.com/
For sleep and meditations
Candlelit Therapy
https://www.livecandlelit.com/
For moms of color
Gotman App:
https://www.gottman.com/couples/apps/
If mom is having issues with her partner
Peanut App
If she talks about feeling alone
Being the only one in her friend group to have a baby
If she just moved
Calm App
If she is having a hard time sleeping
Headspace App
If she is having a hard time sleeping
Insight Timer App
If she is having a hard time sleeping
Dana App
For Spanish Speaking Moms
Free Courses
Mothers and Babies Course
Free and teaches women great skills and techniques
Spanish and English
Favorite Meditations
Loving Kindness
Connecting with Family Members on Behalf of Moms
Care Coordinators can speak with family members to provide resources, like information on upcoming support groups, what symptoms to watch out for, how best to support her, and articles.
Times when we have spoken to a family member it has been by the request of a mom.
My mom would like to talk with you. Is that ok?
We have a link to information, educating them on how best to support her.
Inquire how partners are doing and share resources for them.
1 in 10 dads will experience depression and anxiety after a baby is born, or when their partner experiences a Perinatal Mood and Anxiety Disorder (PMAD).
PSI has a group for dads
Mammha Care Coordinator How To
Mom Screens Positive Now What
You will get notified via an SMS message and email that your patient screened:
Positive
High
(Beginning Care Coordinators will not respond to these URGENT Screens)
URGENT for Self-Harm
(Beginning Care Coordinators will not respond to these URGENT Screens)
You have 24 hours to respond to mom, but sooner is better. Remember what it was like for you. So try to respond to her via text in your Care Coordinator portal within 1 hour.
First response after a positive screen. The goal is to respond back within 1 hour.
Log in to the Care Coordinator portal
Select the patient who just screened positive
Click on her record to review:
Her answers
Check if it looks more like anxiety or depression. Determine if she is crying a lot and/or having issues sleeping
Insurance
This information is necessary to match her with a therapist
Pregnant or Postpartum
If the delivery date is in the future, she is pregnant. Check how far along she is.
If the delivery date is in the past, she is postpartum, also she will have entered a baby/babies names.
Her doctor
Find out who her doctor is in order to respond back to that doctor once you have reached out to the mom
Location of Screen
Check to see if she is remote. If she is remote, she may have called the doctor to say she is not feeling well. If she is in the office, she is likely seeing her doctor at that moment and will not be able to respond to your text immediately.
Initiate first contact from within the portal by clicking on the Conversation button in the top right hand corner of the patient’s screen record.
Note: If you download the patient’s screen report to obtain more information, make sure to delete it immediately after to be HIPAA compliant.
First Contact Via Your Care Coordination Portal
This occurs right after mom screens positive. Initiate a conversation with her from the Care Coordinator portal. This communication will show up on the mom’s phone as a text message.
Your first message should say who you are, that you work with her doctor, that you are here to help support her, and ask what her preference of communication is.
Sample First Contact Message:
“Hi (Name of Mom), My name is (Your Name) and I am a Mammha Care Coordinator. I work with (Name of Provider) to support her/his pregnant and postpartum moms. I see from your recent screen that you may be having a hard time (if it looks like anxiety you can say anxiety, or if she answers she has been crying a lot, you can reference that). I am here to help support you and connect you with the right care.
In the first text to moms, ask whether they prefer communicating by text or by speaking on the phone.
Getting Mom's Communication Preference:
“Do you prefer texting or speaking by phone?
If she says phone, call the mom.
If she says text, continue texting.
If she says phone, it tends to be an initial call then ongoing communication is by text.
If She Does Not Respond To First Outreach Text
If she does not respond to the first text, call her on the phone 24 hours later.
If she does not answer the phone, leave her a voicemail message.
Voicemail Message:
“Hi (Name of Mom), My name is (Your Name) and I am a Mammha Care Coordinator. I work with (Name of Provider) to support her/his pregnant and postpartum moms. I am reaching out because I saw from your recent screen that you may benefit from some resources and extra support. I am here to make sure we get you connected with the right care. You can give me a call back, or I will send a quick text now that you can respond to if that’s easier. Take Care,
Your Name).”
After leaving the voicemail message, return to the Care Coordinator portal, and send her a message. An email may be sent as well, to ensure she receives your information. This is also helpful if she entered her phone number wrong. Her email address is in her screen record.
Follow-Up Text Message After Voicemail:
“Hi (Name of Mom), I just left you a message. I wanted to make sure you have these resources. We have a mom group on Friday at 11 am and we would love to have you. Here is the link. https://www.mammha.com/virtual-support-groups
(If she is pregnant)
Also, here is a workbook for pregnant moms that other moms have found really helpful: https://www.amazon.com/Pregnancy-Workbook-Anxiety-Mindfulness-Techniques-ebook/dp/B091MCMC42
(If she is not pregnant, simply share the support group and the message below)
I can help connect you with a therapist if you want to talk to someone. I’m here to support you.
If she does pick up the phone, share the following:
You are a Mammha Care Coordinator
You work with (Name of the Provider)
You help support her/his pregnant and postpartum moms
According to her recent screen she may benefit from some resources and extra support
You can connect her with the right care
Ask her “How have you been feeling?”
Goal 1: Find out about her symptoms
How are you sleeping?
On a scale of 1 to 10, how are you feeling?
How’s the baby feeding?
How’s the pregnancy going?
How’s your support system?
How are you eating?
Have you been drinking enough water?
Are you taking any time for yourself?
Based on what she shares, listen, affirm what she is saying, and determine any resource/resources to which she can be connected.
Goal 2: Ask if she would be interested in connecting with a therapist who takes her insurance.
Let her know you can help connect her.
Goal 3: Let her know you will get back to her with any resources, therapist, or support group link.
Goal 4: Let her know she is not alone. A Care Coordinator ensures that mom receives the right support.
Goal 5: Let her know if she ever needs someone to talk to she can reach out to you.
After You Reach Mom the First Time: Provider Follow Up
After the first communication with mom, always email the Doctor or Screening Provider back. The goal is to do this within 24 hours. The sooner, the better. Inform the provider that you were able to successfully contact their patient. Only use the patient’s first name, and list any topics that were discussed, and any follow-up details.
Sample Provider Email Message:
Dear Dr. Gaitan,
I have reached out to Katie. We spoke by phone about how to get better sleep, about breastfeeding, and reassuring her it can be hard and it’s normal to feel this way. I am connecting her with a specialized therapist, and will follow up with her to make sure it’s a good match. She received her patient portal, and is also signed up for her automatic supportive SMS messages. I will be following up with her weekly to make sure she feels better.
Thank you for using Mammha.
Maureen
If Mom Does Not Respond to Second Outreach Phone Call or Second Text
If she does not respond to the voicemail message or second text, you need to reach out 24 hours after those attempts (Total time elapsed since she screened positive should be 72 hours)
This will be your final attempt, and it will be via text.
Final Message to Mom If She Does Not Respond to Either Outreach Attempt
Hi (Name of Mom),
Here is the link to your mom portal. I just want to make sure you have it available. It has multiple low and no-cost resources.It has multiple low to no-cost resources, https://www.mammha.com/welcome-master
If you need anything you can always reach out, I am here.
After the third attempt, stop checking in.
If she reaches out to you in the future, you may resume communication and support. You have tried your best. Know that she has her mom portal with resources, and she will receive 90 days of supportive SMS messages.
After Three Attempts with No Contact: Message the Screening Provider
If there has been no response, notify the provider that you attempted to reach mom over the past 3 days, but have not had any response. Also inform them that she has her mom portal, the mom group link was shared, and she is signed up to receive 90 days of supportive SMS messages.
Sample Provider Email Message After No Contact:
Dear Dr. Gaitan,
I want to let you know I tried to reach (Name of Patient - only first name) over the past three days, but have had no luck getting ahold of her. I did share the link to her mom portal with her, a link to our mom group, and she is signed up for Mammha’s 90 days of supportive SMS messages.
Thank you for using Mammha.
Maureen
Suggested Communication and Check-in Timeline for Moms Who Screen Positive
These are the minimum requirements but the Care Coordinator is always the judge. If she sounds like she needs more support, you can always increase your interaction.
Week 1: Three Check-Ins or More
Within 24 hours after screening positive
Introduce yourself
Inquire whether her preference for communication is via text or phon
Goal 1: Determine what her symptoms are.
Try to learn more about what she is feeling. Let her know this information can help find her the best resources.
At this point, locate and identify the best resources for her needs
Ask how she is sleeping,
Ask how she is feeling
Ask about her support system
Ask how the birth was (Birth Trauma)
Goal 2: Inquire if she is interested in connecting with a therapist who takes her insurance.
Goal 3: Be sure to inform her that you will notify her about any resources, therapist, or support group link.
Goal 4: Tell her that she is not alone. Make sure she knows you are there to help her receive the right support.
Goal 5: Make sure she knows if she ever needs someone to talk with she can reach out to you.
Week 1: Check-in 2
Reach out 24 hours after your first check-in to see how she is feeling or sleeping. Bring up something she shared to see if it's getting better, or to let her know that you have a resource that can help.
Week 1: Check-in 3
Ask her, if you helped connect her with a therapist, “Did you get in contact with the therapist?” “Did you schedule a session yet? Remember, I will be following-up to make sure it’s a good match.”
Check-in 4 or 5:
“I want to make sure you have the information for this support group that I think is a great match.” Provide her with the support group information.
Mammha Care Coordinator Check Lists
You can use these checklists to guide you in each interaction depending on where you are in your communication with mom from when she first screened positive.
Week 1
Week 2
Week 3, 4, 5
Week 6
Check out sample transcripts between a Care Coordinator and a positive screened patient.
Mammha Care Coordinator Tool Kit
Cognitive Behavioral Techniques and Coping Skills Toolkit
Mammha Master Tools and Content: www.mammha.com/mammha-master-tools-content
Sleep Techniques for NICU Moms: www.mammha.com/sleep-tips-for-nicu-moms
Circle of Control Activity: www.mammha.com/circle-of-control
Grounding Video: www.mammha.com/grounding
Thoughts Aren’t Facts: www.mammha.com/thoughts-arent-facts
Stop a Worry Cycle Thought: www.mammha.com/stop-a-worry-cycle-with-a-scary-thought
Stop Technique: www.mammha.com/stop-a-worry-cycle-with-a-scary-thought
Ask for What You Need: www.mammha.com/ask-for-what-you-need
Anger and What You Can Do: www.mammha.com/anger
Focus on Your Wins: www.mammha.com/focus-on-your-wins
Breathing 101: www.mammha.com/breathing-101
Focus Only on the Have To’s: www.mammha.com/focus-only-on-the-have-tos
Reframe: www.mammha.com/reframe
Hack Your Brain’s Happiness Chemicals: www.mammha.com/hack-your-brain-chemicals
Boundaries 101: www.mammha.com/boundaries-101
Anger Cool Down Tips: www.mammha.com/anger-tips
Sleep Tips: www.mammha.com/sleep-tips-1
Emotions: www.mammha.com/emotions
Love Bombs: www.mammha.com/love-bombs
Radical Acceptance: www.mammha.com/radical-acceptance
Moms Top 10 Self-Care List: www.mammha.com/moms-top-10-self-care-copy
Five Finger Gratitude Practice: www.mammha.com/5-finger-gratitude-practice
Types of Thoughts: www.mammha.com/types-of-thoughts
Rainbow Breathing: www.mammha.com/rainbow-breathing
Must Knows
Quick Rules
If you do not know the answer to a question, it is ok to say, “I don’t know, let me find out and get back to you”
Always address doctors as Dr.(Name), never their first name.
Always call doctors “Doctor (Name). Even if they use their first name, always say “Dr. (Name) when speaking to them.
Never assume a woman has a husband. Use language like, “your partner.” Wait for them to say what they call their partner.
-Also, it could be a woman. We do not know and do not assume.
Never give advice on taking medicine. We can help support the doctor’s decision to prescribe a particular medication, or her reluctance to take it.
Never cuss
Do not mention god or religion unless they do
Practice active listening
Do not offer to share your story unless it helps them to open up. Be careful not to share any details that could potentially be triggering.
HIPAA
Do not share confidential information.
In emails with the doctor, share only the first name.
If you download a patient record, make sure to delete it.
Do not share phone numbers or contact information with therapists, or resources unless mom gives permission.
Do not share your password with anyone.
What does the EPDS look like?
Edinburgh Postnatal Depression Scale (EPDS)[1]
The questionnaire below is called the Edinburgh Postnatal Depression Scale (EDPS) The EDPS was developed to identify women who may have postpartum depression. Each answer is given a score of 0 to 3 . The maximum score is 30.
Please select the answer that comes closest to how you have felt in the past 7 days:
1. I have been able to laugh and see the funny side of things
As much as I always could
Not quite so much now
Definitely not so much now
Not at all
2. I have looked forward with enjoyment to things
As much as I ever did
Rather less than I used to
Definitely less than I used to
Hardly at all
3. I have blamed myself unnecessarily when things went wrong
Yes, most of the time
Yes, some of the time
Not very often
No, never
4. I have been anxious or worried for no good reason
No, not at all
Hardly ever
Yes, sometimes
Yes, very often
5. I have felt scared or panicky for no very good reason
Yes, quite a lot
Yes, sometimes
No, not much
No, not at all
6. Things have been getting on top of me
Yes, most of the time I haven't been able to cope at all.
Yes, sometimes I haven't been coping as well as usual
No, most of the time I have coped quite well.
No, I have been coping as well as ever.
7. I have been so unhappy that I have had difficulty sleeping
Yes, most of the time
Yes, sometimes
Not very often
No, not at all
8. I have felt sad or miserable
Yes, most of the time
Yes, quite often
Not very often
No, not at all
9. I have been so unhappy that I have been crying
Yes, most of the time
Yes, quite often
Only occasionally
No, never
10. The thought of harming myself has occurred to me